Changes in threat/control-override delusions, substance use, and violence
Main Article Content
Abstract
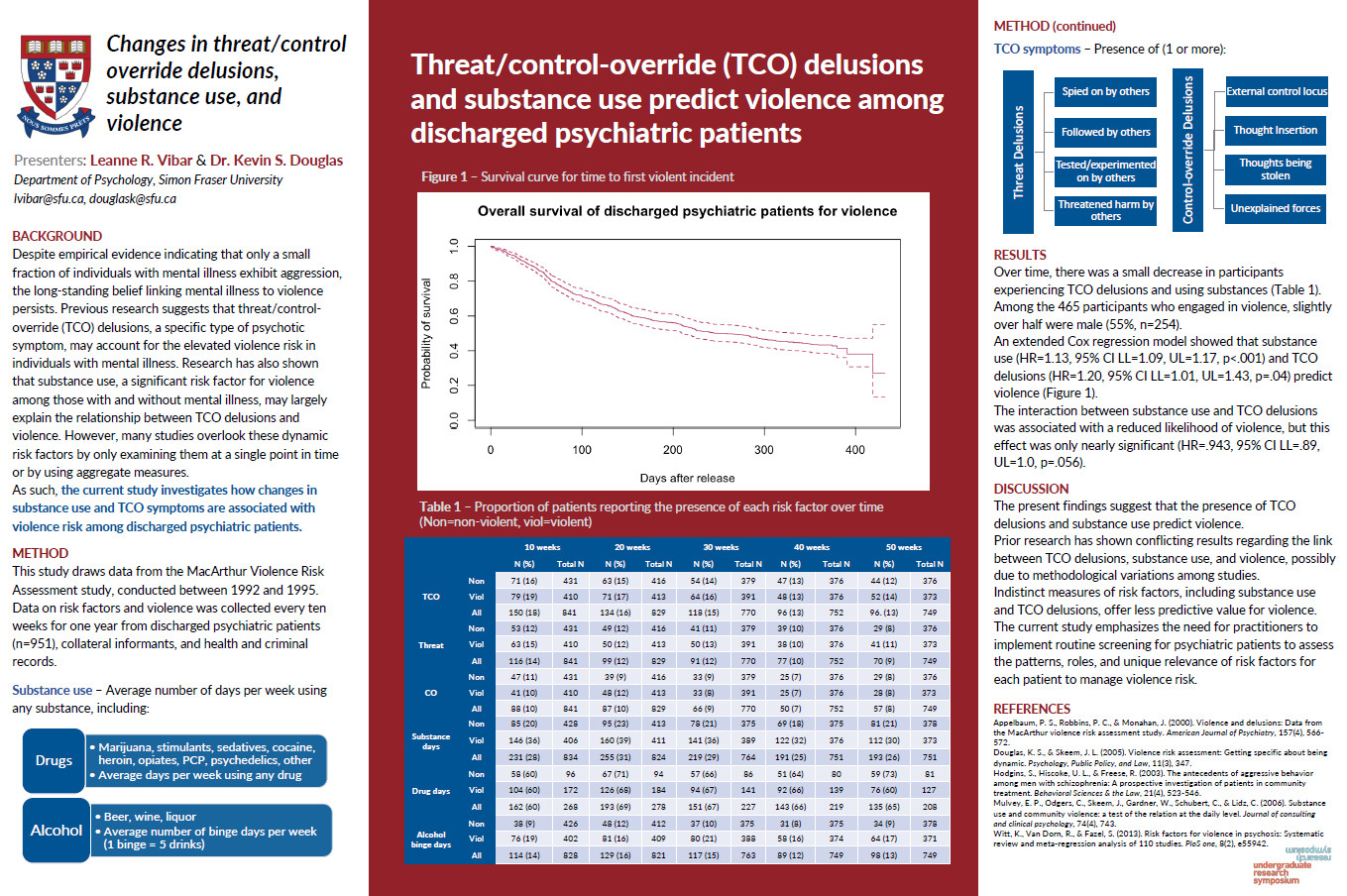
Evidence for an association between major mental illness and violence has grown over the past few decades. However, the specific findings on the nature of this relation vary drastically across studies. Given the increase of patients being treated in community settings, it is important inform appropriate decision-making practices in risk assessment. Several studies have suggested that a specific set of psychotic symptoms, threat/control-override (TCO) delusions, may explain the increased risk of violence among those with mental illness. However, studies have also shown that substance use, a significant risk factor for violence among those with and without mental illness, may largely explain relationship between TCO delusions and violence. To explore this issue, the current study will use data from the MacArthur Risk Assessment study, a prospective, longitudinal study that investigated the risk of violence among discharged psychiatric patients. Identifying and understanding the most significant risk factors is important for informing risk prevention, management, and treatment.
Faculty Supervisor: Dr. Kevin Douglas, Department of Psychology, Simon Fraser University
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
References
Aber, J. L., Brown, J. L., & Jones, S. M. (2003). Developmental trajectories toward violence in
middle childhood: Course, demographic differences, and response to school-based intervention. Developmental Psychology, 39(2), 324.
Adams, S. W., & Yanos, P. T. (2020). Pathways to aggression and violence in psychosis without
longstanding antisocial behavior: A review and proposed psychosocial model for integrative clinical interventions. Psychiatry Research, 293, 113427.
Appelbaum, P. S., Robbins, P. C., & Monahan, J. (2000). Violence and delusions: Data from the
MacArthur violence risk assessment study. American Journal of Psychiatry, 157(4), 566-572.
Baillargeon, J., Penn, J. V., Knight, K., Harzke, A. J., Baillargeon, G., & Becker, E. A. (2010).
Risk of reincarceration among prisoners with co-occurring severe mental illness and substance use disorders. Administration and Policy in Mental Health and Mental Health Services Research, 37, 367-374.
Beaudoin, M., Potvin, S., Dellazizzo, L., Luigi, M., Giguère, C. E., & Dumais, A. (2019).
Trajectories of dynamic risk factors as predictors of violence and criminality in patients discharged from mental health services: A longitudinal study using growth mixture modeling. Frontiers in Psychiatry, 10, 301.
Bentall, R. P., Corcoran, R., Howard, R., Blackwood, N., & Kinderman, P. (2001). Persecutory
delusions: A review and theoretical integration. Clinical Psychology Review, 21(8), 1143-1192.
Bettencourt, B., Talley, A., Benjamin, A. J., & Valentine, J. (2006). Personality and aggressive
behavior under provoking and neutral conditions: A meta-analytic review. Psychological Bulletin, 132(5), 751.
Bjørkly, S. (2002). Psychotic symptoms and violence toward others—a literature review of some
preliminary findings: Part 1. Delusions. Aggression and Violent Behavior, 7(6), 617-631.
Bjørkly, S., Laake, P., Roaldset, J. O., & Douglas, K. S. (2021). The Safe pilot study: A
prospective naturalistic study with repeated measures design to test the psychosis-violence link in and after discharge from forensic facilities. Psychiatry Research, 298, 113793.
Blanchard, A. J. E. (2013). Dynamic risk factors in violence risk assessment: A multiple time-
point evaluation of the HCR-20 and START.
Bo, S., Abu-Akel, A., Kongerslev, M., Haahr, U. H., & Simonsen, E. (2011). Risk factors for
violence among patients with schizophrenia. Clinical Psychology Review, 31(5), 711-726.
Boles, S. M., & Miotto, K. (2003). Substance abuse and violence: A review of the
literature. Aggression and Violent Behavior, 8(2), 155-174.
British Columbia Mental Health Act. (2023). Mental Health Act. Retrieved from the British
Columbia Mental Health Act. Website: https://www.bclaws.gov.bc.ca/civix/document/id/complete/statreg/00_96288_01
Buckley, P. F., & Meyer, J. M. (2009). Substance abuse and schizophrenia. Medical Illness and
Schizophrenia, 275-302.
Cafferky, B. M., Mendez, M., Anderson, J. R., & Stith, S. M. (2018). Substance use and intimate
partner violence: A meta-analytic review. Psychology of Violence, 8(1), 110.
Cerdá, M., Bordelois, P. M., Keyes, K. M., Galea, S., Koenen, K. C., & Pardini, D. (2013).
Cumulative and recent psychiatric symptoms as predictors of substance use onset: Does timing matter?. Addiction, 108(12), 2119-2128.
Chadwick, N. C. (2014). Validating the Dynamic Risk Assessment for Offender Re-entry
(DRAOR) in a sample of US probationers and parolees (Doctoral dissertation, Carleton University).
Chermack, S. T., & Blow, F. C. (2002). Violence among individuals in substance abuse
treatment: The role of alcohol and cocaine consumption. Drug and Alcohol Dependence, 66(1), 29-37.
Coid, J. W., Ullrich, S., Bebbington, P., Fazel, S., & Keers, R. (2016). Paranoid ideation and
violence: Meta-analysis of individual subject data of 7 population surveys. Schizophrenia Bulletin, 42(4), 907-915.
Combs, D. R., Penn, D. L., Michael, C. O., Basso, M. R., Wiedeman, R., Siebenmorgan, M.,
Tiegreen, J., & Chapman, D. (2009). Perceptions of hostility by persons with and without persecutory delusions. Cognitive Neuropsychiatry, 14(1), 30–52. https://doi.org/10.1080/13546800902732970
Criminal Code, R.S.C., 1985, c. C-46, s. 16. (2023). Retrieved from: https://laws-
lois.justice.gc.ca/eng/acts/C-46/FullText.html?
de Vries Robbé, M., Vogel, V. D., & Douglas, K. S. (2013). Risk factors and protective factors: A
two-sided dynamic approach to violence risk assessment. Journal of Forensic Psychiatry & Psychology, 24(4), 440-457.
de Vries Robbé, M., De Vogel, V., Douglas, K. S., & Nijman, H. L. (2015). Changes in dynamic
risk and protective factors for violence during inpatient forensic psychiatric treatment: Predicting reductions in post discharge community recidivism. Law and Human Behavior, 39(1), 53.
Doran, N., Luczak, S. E., Bekman, N., Koutsenok, I., & Brown, S. A. (2012). Adolescent
substance use and aggression: A review. Criminal Justice and Behavior, 39(6), 748-769.
Douglas, K. S., Ogloff, J. R., Nicholls, T. L., & Grant, I. (1999). Assessing risk for violence
among psychiatric patients: The HCR-20 violence risk assessment scheme and the Psychopathy Checklist: Screening Version. Journal of Consulting and Clinical psychology, 67(6), 917.
Douglas, K. S., & Skeem, J. L. (2005). Violence risk assessment: Getting specific about being
dynamic. Psychology, Public Policy, and Law, 11(3), 347.
Douglas, K. S., Guy, L. S., & Hart, S. D. (2009). Psychosis as a risk factor for violence to others:
A meta-analysis. Psychological Bulletin, 135(5), 679.
Douglas, K. S., Hart, S. D., Webster, C. D., Belfrage, H., Guy, L. S., & Wilson, C. M. (2014).
Historical-clinical-risk management-20, version 3 (HCR-20V3): Development and overview. International Journal of Forensic Mental Health, 13(2), 93-108.
Douglas, K. S., & Shaffer, C. S. (2020). The science of and practice with the HCR-20 V3
(historical-clinical-risk management-20, version 3). In Handbook of violence risk assessment (pp. 253-293). Routledge.
Elbogen, E. B., & Johnson, S. C. (2009). The intricate link between violence and mental
disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 66(2), 152-161.
Fanning, J. R., Berman, M. E., Mohn, R. S., & McCloskey, M. S. (2011). Perceived threat
mediates the relationship between psychosis proneness and aggressive behavior. Psychiatry Research, 186(2-3), 210-218.
Fazel, S., Bains, P., & Doll, H. (2006). Substance abuse and dependence in prisoners: A
systematic review. Addiction, 101(2), 181-191.
Fazel, S., Smith, E. N., Chang, Z., & Geddes, J. R. (2018). Risk factors for interpersonal violence: an
umbrella review of meta-analyses. The British Journal of Psychiatry, 213(4), 609-614.
Feingold, A., Kerr, D. C., & Capaldi, D. M. (2008). Associations of substance use problems with
intimate partner violence for at-risk men in long-term relationships. Journal of Family Psychology, 22(3), 429.
Freeman, D. (2016). Persecutory delusions: A cognitive perspective on understanding and
treatment. The Lancet Psychiatry, 3(7), 685-692.
Garson, G. D. (2013). Fundamentals of hierarchical linear and multilevel modeling. Hierarchical
linear modeling: Guide and applications, 3-25.
Green, B., Schramm, T. M., Chiu, K., McVie, N., & Hay, S. (2009). Violence severity and
psychosis. International Journal of Forensic Mental Health, 8(1), 33-40.
Greenfeld, L. A., & Henneberg, M. A. (2001). Victim and offender self-reports of alcohol
involvement in crime. Alcohol Research & Health, 25(1), 20.
Greiner, L. E., Law, M. A., & Brown, S. L. (2015). Using dynamic factors to predict recidivism
among women: A four-wave prospective study. Criminal Justice and Behavior, 42(5), 457-480.
Gregg, L., Barrowclough, C., & Haddock, G. (2007). Reasons for increased substance use in
psychosis. Clinical Psychology Review, 27(4), 494-510.
Grisso, T., Davis, J., Vesselinov, R., Appelbaum, P. S., & Monahan, J. (2000). Violent thoughts
and violent behavior following hospitalization for mental disorder. Journal of Consulting and Clinical Psychology, 68(3), 388.
Heimer, K. (1997). Socioeconomic status, subcultural definitions, and violent
delinquency. Social Forces, 75(3), 799-833.
Harris, M. N., & Teasdale, B. (2021). The prediction of repeated violence among individuals
with serious mental disorders: Situational versus dispositional factors. Journal of Interpersonal Violence, 36(1-2), 691-721.
Hodgins, S., Hiscoke, U. L., & Freese, R. (2003). The antecedents of aggressive behavior among
men with schizophrenia: A prospective investigation of patients in community treatment. Behavioral Sciences & the Law, 21(4), 523-546.
Hodgins, S. (2008). Violent behaviour among people with schizophrenia: A framework for
investigations of causes, and effective treatment, and prevention. Philosophical Transactions of the Royal Society B: Biological Sciences, 363(1503), 2505-2518.
Hogan, N. R., & Olver, M. E. (2019). Static and dynamic assessment of violence risk among
discharged forensic patients. Criminal Justice and Behavior, 46(7), 923-938.
Horney, J., Osgood, D. W., & Marshall, I. H. (1995). Criminal careers in the short-term: Intra-
individual variability in crime and its relation to local life circumstances. American Sociological Review, 655-673.
Houser, K. A., Belenko, S., & Brennan, P. K. (2012). The effects of mental health and substance
abuse disorders on institutional misconduct among female inmates. Justice Quarterly, 29(6), 799-828.
Johnson, K. L., Desmarais, S. L., Grimm, K. J., Tueller, S. J., Swartz, M. S., & Van Dorn, R. A.
(2016). Proximal risk factors for short-term community violence among adults with mental illnesses. Psychiatric Services, 67(7), 771-778.
Junginger, J., Parks-Levy, J., & McGuire, L. (1998). Delusions and symptom-consistent
violence. Psychiatric Services, 49(2), 218-220.
Kamimura, A., Yoshihama, M., & Bybee, D. (2013). Trajectory of intimate partner violence and
healthcare seeking over the life course: Study of Japanese women in the Tokyo metropolitan area, Japan. Public Health, 127(10), 902-907.
Keers, R., Ullrich, S., DeStavola, B. L., & Coid, J. W. (2014). Association of violence with
emergence of persecutory delusions in untreated schizophrenia. American Journal of Psychiatry, 171(3), 332-339.
Kennedy, P., Clarke, G., O’Neill, A., Groeger, J. A., Eamonn Martin Quigley, Shanahan, F., Cryan, J. F., & Dinan, T. G. (2013). Cognitive performance in irritable bowel syndrome: evidence of a stress-related impairment in visuospatial memory. Psychological Medicine, 44(7), 1553–1566. https://doi.org/10.1017/s0033291713002171
Kim, D., Brown, E., Reynolds, S., Geros, H., Sizer, H., Tindall, R., McGorry, P. D., & O’Donoghue, B. (2019). The rates and determinants of disengagement and subsequent re-engagement in young people with first-episode psychosis. Social Psychiatry and Psychiatric Epidemiology, 54(8), 945–953. https://doi.org/10.1007/s00127-019-01698-7
Kivisto, A. J., & Watson, M. E. (2016). 12-month prevalence, trends, gender differences, and the impact of mental health services on intimate partner violence perpetration among discharged psychiatric inpatients. Journal of Family Violence, 31, 379-385.
Lambe, S., Cooper, K., Fazel, S., & Freeman, D. (2023). Psychological framework to understand
interpersonal violence by forensic patients with psychosis. The British Journal of Psychiatry, 1-8.
Lamsma, J., & Harte, J. M. (2015). Violence in psychosis: Conceptualizing its causal relationship
with risk factors. Aggression and Violent Behavior, 24, 75-82.
Lamsma, J. (2019). Risk factors for violent behaviour in psychotic disorders: Substance use and
cognition (Doctoral dissertation, University of Oxford).
Lidz, C. W., Mulvey, E. P., & Gardner, W. (1993). The accuracy of predictions of violence to
others. JAMA, 269(8), 1007-1011.
Link, B. G., Andrews, H., & Cullen, F. T. (1992). The violent and illegal behavior of mental
patients reconsidered. American Sociological Review, 275-292.
Link, B., Stueve, A. (1994) Psychotic symptoms and the violent/illegal behavior of mental
patients compared to community controls. In: Monahan J, Steadman H (eds) Violence and mental disorder. University of Chicago Press, Chicago, pp 137-160
Link, B. G., Stueve, A., & Phelan, J. (1998). Psychotic symptoms and violent behaviors: Probing
the components of “threat/control-override” symptoms. Social Psychiatry and Psychiatric Epidemiology, 33, S55-S60.
Link, B. G., Monahan, J., Stueve, A., & Cullen, F. T. (1999). Real in their consequences: A
sociological approach to understanding the association between psychotic symptoms and violence. American Sociological Review, 316-332.
Mojtabai, R. (2006). Psychotic-like experiences and interpersonal violence in the general
population. Social Psychiatry and Psychiatric Epidemiology, 41, 183-190.
Monahan, J., Steadman, H. J., Silver, E., Appelbaum, P. S., Robbins, P. C., Mulvey, E. P., ... & Banks, S. (2001). Rethinking risk assessment: The MacArthur study of mental disorder and
violence. Oxford University Press.
Mulvey, E. P., Gardner, W., Lidz, C. W., & Shaw, E. C. (1996). Clinical versus actuarial
predictions of violence in patients with mental illnesses. Journal of Consulting and Clinical Psychology, 64(3), 602.
Mulvey, E. P., Odgers, C., Skeem, J., Gardner, W., Schubert, C., & Lidz, C. (2006). Substance
use and community violence: a test of the relation at the daily level. Journal of consulting and clinical psychology, 74(4), 743.
Oliveira, R. V., & Beaver, K. M. (2020). Association between self-reported traumatic brain injury
and threat/control-override. International Journal of Forensic Mental Health, 19(2), 152-164.
Oyebode, F. (2018). Sims' symptoms in the mind: Textbook of descriptive psychopathology.
Elsevier Health Sciences.
Patel, A., Barot, C. K., Vankar, G., & Pal, S. (2019). Acting on delusions in patients suffering
from schizophrenia. Archives of Psychiatry and Psychotherapy, 21(4), 52-61.
Penney, S. R., Marshall, L. A., & Simpson, A. I. (2016). The assessment of dynamic risk among
forensic psychiatric patients transitioning to the community. Law and Human Behavior, 40(4), 374.
Perälä, J., Suvisaari, J., Saarni, S. I., Kuoppasalmi, K., Isometsä, E., Pirkola, S., Partonen, T., Tuulio‐Henriksson, A., Hintikka, J., Kieseppä, T., Härkänen, T., Koskinen, S., & Lönnqvist, J. (2007). Lifetime Prevalence of Psychotic and Bipolar I Disorders in a General Population. Archives of General Psychiatry, 64(1), 19–19. https://doi.org/10.1001/archpsyc.64.1.19
Palmstierna, T., & Olsson, D. (2007). Violence from young women involuntarily admitted for
severe drug abuse. Acta Psychiatrica Scandinavica, 115(1), 66-72.
Redman, S. (2021). The effect of threat control-override on the relation between psychosis-risk
symptoms and aggression in help-seeking adolescents (Doctoral dissertation, University of Maryland, Baltimore County).
Robins, L. N. (1981). National Institute of Mental Health Diagnostic Interview Schedule. Archives of General Psychiatry, 38(4), 381–381. https://doi.org/10.1001/archpsyc.1981.01780290015001
Sacks, S., Cleland, C. M., Melnick, G., Flynn, P. M., Knight, K., Friedmann, P. D., Prendergast, M., & Coen, C. (2009). Violent offenses associated with co-occurring substance use and mental health problems: Evidence from CJDATS. Behavioral Sciences & the Law, 27(1), 51–69. https://doi.org/10.1002/bsl.850
Silver, E., Piquero, A. R., Jennings, W. G., Piquero, N. L., & Leiber, M. (2011). Assessing the violent offending and violent victimization overlap among discharged psychiatric patients. Law and Human Behavior, 35, 49-59.
Silverstein, S. M., Del Pozzo, J., Roché, M., Boyle, D., & Miskimen, T. (2020). Schizophrenia
and violence: Realities and recommendations. Reviewing Crime Psychology, 181-202.
Skeem, J. L., & Mulvey, E. P. (2001). Psychopathy and community violence among civil
psychiatric patients: Results from the MacArthur Violence Risk Assessment Study. Journal of Consulting and Clinical Psychology, 69(3), 358.
Skeem, J. L., Monahan, J., & Mulvey, E. P. (2002). Psychopathy, treatment involvement, and
subsequent violence among civil psychiatric patients. Law and Human Behavior, 26, 577-603.
Skeem, J. L., Schubert, C., Odgers, C., Mulvey, E. P., Gardner, W., & Lidz, C. (2006).
Psychiatric symptoms and community violence among high-risk patients: A test of the relationship at the weekly level. Journal of Consulting and Clinical Psychology, 74(5), 967.
Skeem, J., Kennealy, P., Monahan, J., Peterson, J., & Appelbaum, P. (2016). Psychosis
uncommonly and inconsistently precedes violence among high-risk individuals. Clinical Psychological Science, 4(1), 40-49.
Steadman, H. J., Mulvey, E. P., Monahan, J., Pamela Clark Robbins, Appelbaum, P. S., Grisso, T., Roth, L. H., & Silver, E. (1998). Violence by People Discharged From Acute Psychiatric Inpatient Facilities and by Others in the Same Neighborhoods. Archives of General Psychiatry, 55(5), 393–393. https://doi.org/10.1001/archpsyc.55.5.393
Stompe, T., Ortwein-Swoboda, G., & Schanda, H. (2004). Schizophrenia, delusional symptoms,
and violence: The threat/control-override concept reexamined. Schizophrenia Bulletin, 30(1), 31-44.
Straus, M. A. (1990). (1990a). The Conflict Tactics Scales and its critics: An evaluation and new
data on validity and reliability. In MA Straus & RJ Gelles (Eds.), Physical violence in American families: Risk factors and adaptations to violence in 8,145 families (pp. 49-73). New Brunswick, NJ: Transaction Publishing.
Swanson, J. W., Holzer III, C. E., Ganju, V. K., & Jono, R. T. (1990). Violence and psychiatric disorder in the community: Evidence from the Epidemiologic Catchment Area surveys. Psychiatric Services, 41(7), 761-770.
Swanson, J. W., Borum, R., Swartz, M. S., & Monahan, J. (1996). Psychotic symptoms and disorders and the risk of violent behaviour in the community. Criminal Behaviour and Mental Health, 6(4), 309-329.
Swanson, J. W., Swartz, M. S., Van, R. A., Elbogen, E. B., H. Ryan Wagner, Rosenheck, R. A., T. Scott Stroup, McEvoy, J. P., & Lieberman, J. A. (2006). A national study of violent behavior in persons with schizophrenia. Archives of General Psychiatry, 63(5), 490–490. https://doi.org/10.1001/archpsyc.63.5.490
Teasdale, B., Silver, E., & Monahan, J. (2006). Gender, threat/control-override delusions and violence. Law and Human Behavior, 30(6), 649.
Torres, F. (2020). What is Schizophrenia? American Psychiatric Association. https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia
van der Kraan, J., Verkes, R. J., Goethals, K., Vissers, A., Brazil, I., & Bulten, E. (2014). Substance use disorders in forensic psychiatric patients. International Journal of Law and Psychiatry, 37(2), 155-159.
Volavka, J., & Citrome, L. (2011). Pathways to aggression in schizophrenia affect results of treatment. Schizophrenia Bulletin, 37(5), 921-929.
Walsh, E., Gilvarry, C., Chiara Samele, Harvey, K., Manley, C., T. Tattan, Tyrer, P., Creed, F., Murray, R. M., & Fahy, T. (2004). Predicting violence in schizophrenia: A prospective study. Schizophrenia Research, 67(2-3), 247–252. https://doi.org/10.1016/s0920-9964(03)00091-4
Witt, K., Van Dorn, R., & Fazel, S. (2013). Risk factors for violence in psychosis: Systematic
review and meta-regression analysis of 110 studies. PloS one, 8(2), e55942.
Woltman, H., Feldstain, A., MacKay, J. C., & Rocchi, M. (2012). An introduction to hierarchical
linear modeling. Tutorials in Quantitative Methods for Psychology, 8(1), 52-69.
World Health Organization. (2022). World Health Organization Violence Prevention Unit:
Approach, objectives, and activities. World Health Organization. https://cdn.who.int/media/docs/default-source/documents/social-determinants-of-health/who_2022_plv_strategy_2022-2026_finalfile.pdf?sfvrsn=c819ff54_3
Yang, S., Mulvey, E. P., Loughran, T. A., & Hanusa, B. H. (2012). Psychiatric symptoms and
alcohol use in community violence by persons with a psychotic disorder or depression. Psychiatric Services, 63(3), 262-269.